Welcome to our in-depth exploration of CPT placement of wound vac, a procedure that revolutionizes wound care. Join us as we delve into the intricacies of this technique, examining its nuances and unraveling its complexities. Our journey begins with understanding the appropriate CPT code for wound vac placement, a crucial step in ensuring accurate reimbursement.
As we progress, we will explore the factors that influence CPT code selection, providing real-world examples to solidify your understanding. We will then guide you through the step-by-step procedure for wound vac placement, ensuring that you have a clear roadmap for successful implementation.
CPT Placement of Wound Vac

The appropriate CPT code for placement of a wound vac is determined by several factors, including the type of wound vac, the size of the wound, and the location of the wound. In general, the following CPT codes are used for wound vac placement:
- 97605: Placement of a simple wound vac
- 97606: Placement of a complex wound vac
- 97607: Placement of a wound vac with instillation and/or irrigation
The following are some examples of different scenarios and the corresponding CPT codes:
- Placement of a simple wound vac on a small wound on the leg: 97605
- Placement of a complex wound vac on a large wound on the chest: 97606
- Placement of a wound vac with instillation and irrigation on a wound on the abdomen: 97607
Procedure for Wound Vac Placement

Wound vac placement involves several key steps to ensure proper application and effectiveness.
Patient Preparation
Prior to wound vac placement, the patient should be adequately prepared to minimize discomfort and optimize the procedure’s success. This includes:
- Obtaining informed consent from the patient.
- Assessing the patient’s pain level and administering appropriate pain medication.
- Positioning the patient comfortably to provide optimal access to the wound site.
- Cleaning the wound site thoroughly to remove any debris or exudate.
Wound Preparation
Once the patient is prepared, the wound site should be carefully prepared to ensure proper adhesion and functioning of the wound vac. This involves:
- Trimming any excess skin or tissue around the wound edges.
- Debriding the wound to remove any necrotic tissue or foreign bodies.
- Irrigating the wound with sterile saline to remove any debris or bacteria.
- Drying the wound site thoroughly with sterile gauze.
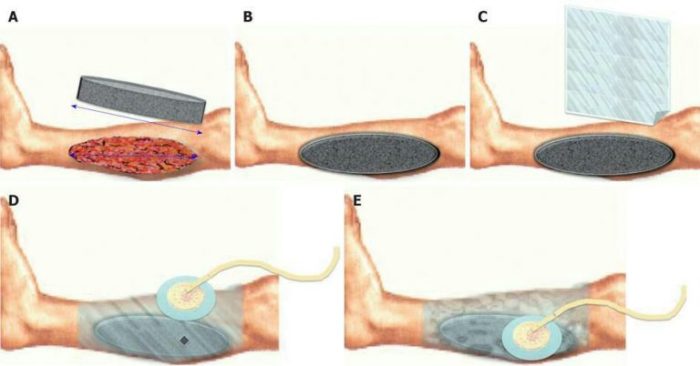
Device Application
With the wound site properly prepared, the wound vac device can be applied. This involves:
- Placing the wound vac sponge or dressing over the wound site.
- Securing the sponge or dressing with the appropriate dressing materials.
- Connecting the wound vac tubing to the sponge or dressing.
- Setting the wound vac to the appropriate suction level.
- Monitoring the wound vac for proper functioning and any signs of infection or complications.
| Step | Description |
|---|---|
| Patient Preparation | Obtain consent, manage pain, position patient, clean wound site |
| Wound Preparation | Trim excess tissue, debride wound, irrigate and dry |
| Device Application | Place sponge/dressing, secure, connect tubing, set suction |
| Monitoring | Check function, monitor for infection/complications |
Post-Placement Care and Monitoring
After wound vac placement, proper care and monitoring are crucial to ensure optimal healing and prevent complications. Regular dressing changes, wound assessments, and patient education are essential aspects of post-placement care.
Frequency and Type of Dressing Changes
Dressing changes are typically performed every 2-3 days, depending on the wound condition and drainage. The type of dressing used will vary based on the wound characteristics, such as exudate amount, infection risk, and tissue type.
- Foam dressings:Absorbant and conformable, suitable for low to moderate exudate wounds.
- Alginate dressings:Highly absorbent and hemostatic, ideal for heavily draining wounds.
- Hydrocolloid dressings:Self-adhesive and moisture-retentive, promoting autolytic debridement.
- Transparent film dressings:Waterproof and semi-permeable, allowing for wound visualization without dressing removal.
Potential Complications and Management
Despite proper care, complications can occasionally occur with wound vac therapy. These include:
- Infection:Monitor for signs of infection, such as redness, swelling, pain, or foul odor. Antibiotics may be prescribed if infection is suspected.
- Leakage:Ensure the wound vac is properly sealed to prevent leakage, which can lead to maceration or infection.
- Skin irritation:The adhesive used to secure the dressing may cause skin irritation. Use hypoallergenic dressings and apply barrier cream to surrounding skin.
- Pain:Wound vac therapy can cause discomfort, especially during dressing changes. Provide pain medication and ensure the dressing is not too tight.
Documentation and Billing

Proper documentation and accurate billing are crucial for wound vac placement procedures. Detailed records ensure effective patient care, accurate reimbursement, and legal protection.
While the proper placement of a wound vac is crucial for effective healing, if you find yourself in a pinch and need a comprehensive guide to the upcoming AP Gov midterm, look no further than this ap gov midterm study guide . Rest assured, once you’ve aced that exam, you can return to perfecting your wound vac placement techniques with renewed vigor.
Documentation Requirements
- Patient’s medical history and current condition
- Wound assessment and characteristics (size, depth, location, drainage)
- Rationale for wound vac placement
- Type of wound vac used
- Placement technique and settings
- Frequency and duration of dressing changes
- Monitoring parameters (e.g., wound healing, infection control)
- Patient education and instructions
- Follow-up plan and expected outcomes
Sample Progress Note Template
Date:
Patient Name:
Wound Assessment:
Wound Vac Placement:
- Type of wound vac:
- Placement technique:
- Settings:
Frequency and Duration of Dressing Changes:
Monitoring Parameters:
Patient Education and Instructions:
Follow-up Plan:
Expected Outcomes:
Billing Process
Wound vac placement is typically billed using the following codes:
- CPT code 97605: Wound vac placement, initial
- CPT code 97606: Wound vac placement, subsequent
Reimbursement varies depending on insurance coverage, but typically includes payment for the device, supplies, and nursing care.
Comparison to Other Wound Management Techniques
Wound vac placement is a widely used technique for managing wounds. However, it’s important to compare it to other available wound management techniques to make informed decisions about the best approach for each patient.
Two common alternative techniques are negative pressure wound therapy (NPWT) and moist wound healing.
Negative Pressure Wound Therapy (NPWT), Cpt placement of wound vac
- Involves applying a vacuum dressing to the wound, creating negative pressure that promotes fluid drainage and wound contraction.
- Advantages:
- Promotes faster wound healing.
- Reduces infection risk.
- Disadvantages:
- Can be more expensive than other techniques.
- May cause discomfort or pain.
Moist Wound Healing
- Aims to create a moist environment around the wound, which promotes natural healing processes.
- Advantages:
- Promotes faster healing.
- Reduces scarring.
- Disadvantages:
- May require more frequent dressing changes.
- May increase infection risk if not managed properly.
Key Differences
- Mechanism of action:Wound vac placement uses suction to remove fluids and promote healing, while NPWT uses negative pressure to create a vacuum environment, and moist wound healing relies on a moist environment.
- Cost:Wound vac placement is typically more expensive than moist wound healing but less expensive than NPWT.
- Comfort:Wound vac placement can be uncomfortable, while moist wound healing is generally more comfortable.
- Effectiveness:All three techniques can be effective in promoting wound healing, but the best choice depends on the specific wound and patient.
Special Considerations

Wound vac placement requires special considerations for specific patient populations, such as pediatric patients, geriatric patients, and patients with comorbidities.
Pediatric Patients
Pediatric patients have delicate skin and smaller body size, which require careful device selection and placement.
- Use smaller wound vac devices designed for pediatric use.
- Place the device gently to avoid skin irritation.
- Monitor the patient closely for any signs of discomfort or complications.
Geriatric Patients
Geriatric patients may have fragile skin and underlying health conditions that require special attention.
- Use low-pressure settings to avoid tissue damage.
- Consider using dressings that protect the skin from irritation.
- Monitor the patient closely for any signs of infection or other complications.
Patients with Comorbidities
Patients with comorbidities, such as diabetes or obesity, may require additional care during wound vac placement.
- Control blood sugar levels in diabetic patients to reduce the risk of infection.
- Use devices that can accommodate larger wounds in obese patients.
- Monitor the patient closely for any signs of pressure ulcers or other complications.
Expert Answers: Cpt Placement Of Wound Vac
What is the most common CPT code for wound vac placement?
The most common CPT code for wound vac placement is 97606.
How often should dressing changes be performed after wound vac placement?
Dressing changes should be performed every 2-3 days, or as directed by the healthcare provider.
What are the potential complications of wound vac placement?
Potential complications include infection, bleeding, and skin irritation.